The COVID-19 pandemic is demanding swift adaptability from us all – parents and teachers, restaurants and retail, and, of course, all aspects of our health care infrastructure. Some of the most surprising examples of adaptability come from health insurers, who acted quickly to put people first. They waived cost sharing for testing and treatment. They expanded access to telehealth and virtual care. They adapted to care provider needs for payment and protocols, and they gave time, money and resources to support local communities and vulnerable populations.

These actions fly in the face of the perceptions many health consumers have of insurers. However, recent research from Ketchum’s Brand Reckoning 2020 study suggests the people-first actions of health insurers have not only been valuable in addressing the public health crisis, but also caused perceptions to shift and an unexpected reputation halo to form.
Improved Industry Perception
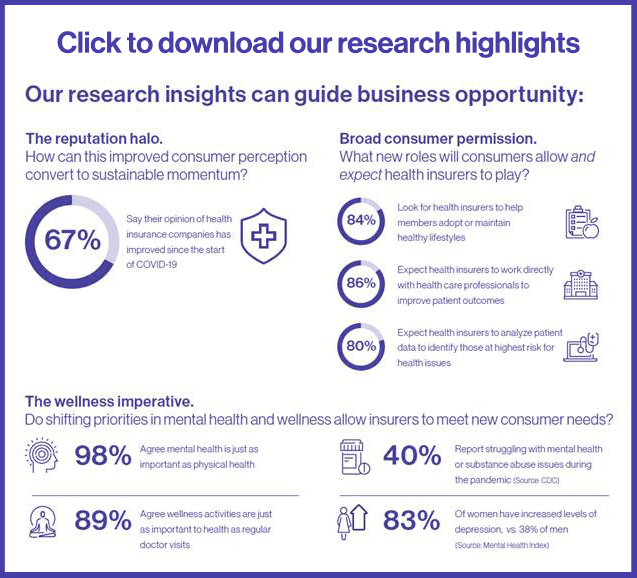
Ketchum’s survey of more than 4,000 Americans showed a surprising 67% say their opinion of health insurance companies has improved since the start of the COVID crisis. This speaks not only to the operational actions many insurers took, but also the way insurers communicated information, listened to their health consumers and became a trusted source of information and support.
I recently hosted a client panel discussion with communications leaders from several top health insurers around the country: Anthem, Inc.; Blue Cross and Blue Shield of North Carolina; and Horizon Blue Cross Blue Shield of New Jersey. As part of that discussion, David Kochman, vice president of communications at Blue Cross and Blue Shield of North Carolina, highlighted the critical importance of proactive engagement. During the onset of the pandemic when confusion spread quickly, Blue NC took the opportunity to deliver the message directly to consumers, leveraging a diverse set of communication channels to engage and provide the tools and resources needed to inform health and wellness decisions.
Expectation to Deliver on Evolving Consumer Needs
At the same time as consumers’ perception of insurers has shifted upward, expectations for the role insurers can play in consumer health has broadened. Ketchum’s research found more than 4 in 5 Americans are looking for health insurance companies to be more involved with providing ways for members to adopt or maintain healthy behaviors. This includes working directly with care providers, supporting healthy behaviors, and utilizing health data to proactively identify at-risk individuals.
For many insurers, this presents an opportunity to showcase and extend work they have already been pioneering. As Jill Becher, vice president for public relations at Anthem, Inc., noted during our discussion, insurers like many in the BCBS network have been innovating health and wellness resources for many years. Organizations like Anthem recognize factors such as mental and behavioral health, access to food, housing and transportation and other social drivers are critical in the whole health of an individual. These factors also have significant impact on outcomes, access and cost. And as such, progressive employers invest in programs as part of member benefits and in community action to make a difference. Placing a greater focus and an increased access to these tools can help meet a growing consumer demand.
Maintaining the Reputation Halo
The challenge now, of course, is to understand how to continue to meet, maintain, and even build on this recently bestowed reputation halo. Tom Wilson, director of public affairs for Horizon Blue Cross New Jersey, pointed out the following in our discussion: while much of how insurers act and are perceived will depend on the ongoing evolution of this public health crisis, the past six months have demonstrated there is a role to be proactive and engage consumers in a trusted manner.
Tom also acknowledges in order to achieve meaningful improvements in brand reputation, leaders must attach the same value to actions supporting their company’s reputation as they do financial, human capital and operations. By doing so, health care organizations can act and communicate in a way that meets consumer expectations and earns their trust.
Ketchum would like to acknowledge the insights and participation of Jill Becher, David Kochman, and Tom Wilson in our client panel discussion. To view a recording of the panel, please register here. For more information on Ketchum’s Brand Reckoning 2020 research or to discuss your brand’s reputation maturity, please reach out to Kelly Calabria.